Walking Past that Homeless Guy
Peter, pictured above with interviewer (his consent was obtained to publish photo)
Homelessness and Complex needs – Fulfilling Lives in Islington and Camden
By Nikki Francalanza
7,500 people sleep rough on the streets of London every year (1), a figure that has more than doubled in five years according to the latest figures and statistics from the Combined Homelessness and Information Network CHAIN (2). They come from every walk of life, and many of them want to find work. We want to challenge the perception that homeless people are any different from the rest of us. Homelessness begins when something bad happens and you don’t have family or friends around to help. It could happen to any of us. Relationship breakdown, redundancy, poor mental health, alcohol/substance addiction, domestic abuse – these are just some of the reasons why people end up homeless.
By and large, people don’t choose to be homeless – they find themselves sleeping on the street because they are facing a major crisis that means they’ve ended up with nowhere else to stay. Homelessness comes in a variety of forms, and may also include people whose primary night-time residence is in a homeless shelter, a warming centre, a domestic violence shelter, a vehicle, squatting, cardboard boxes, a tent, tarpaulins, or other ad hoc housing situations. A home is not just a physical space: it provides roots, identity, security, a sense of belonging and a place of emotional wellbeing.
The rise in homelessness is being put down to a number of factors. These include cuts to council funding meaning that many local authorities struggle to accommodate people in need, housing benefit cuts, lack of affordable housing, cuts to mental health services that leave many vulnerable people with nowhere to go, a growing number of people coming from the EU to find work who end up sleeping rough after being exploited by employers. With the general situation and potentially more government funding cuts on the horizon it is difficult to see how there will be any future improvement. If the situation prevails, then the numbers forced to sleep rough will continue to rise and more evictions of vulnerable people will be inevitable.
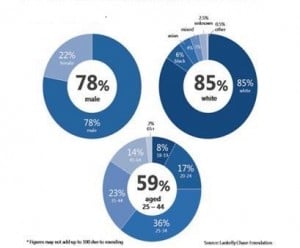
But what do we mean by homelessness and complex needs? Also termed as multiple exclusion homelessness, it’s the extreme end of homelessness – often associated with chaotic lifestyles, repeat homelessness, experience of drug or alcohol dependency, mental health issues, criminality/anti-social behaviour (ASB) issues, and rough sleeping. In terms of demographics, those with the most complex needs are predominantly male (78%), white (85%) and aged between 25 and 44 (59%)(3) (Figure 1). Having to face the reality of life without a stable home, often makes these problems worse. In order to address these needs, individuals require intensive support, not just a roof over their heads.
Figure 1
Fulfilling Lives in Islington and Camden (FLIC)
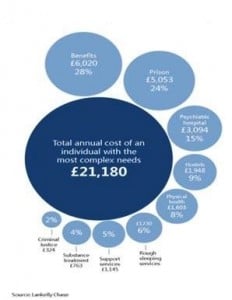
Figure 2
FLIC is an 8 year Big Lottery funded project run by Single Homeless Project (SHP), which aims to improve the stability, confidence and capability of people with multiple and complex needs to lead better lives as a result of timely, supportive and coordinated services. The project works intensively with around 120 people a year, all of whom have complex, unmet needs in all of the four following areas: mental ill health, alcohol and/or drug use, offending behaviour and homelessness. All of these people are those who have so far fallen through the cracks between services due to the multiple and complex nature of their needs, and because no one service takes overall responsibility for helping them to deal with all their issues systematically.
The FLIC team is made up of nine highly experienced local specialist link workers who have been seconded to SHP from three project delivery partners (St. Mungo’s Broadway, Crime Reduction Initiative – CRI, Providence Row). Specialisms include mental health, substance use, criminal justice, housing/homelessness and physical health. The approach taken by the FLIC team focuses on making maximum use of the existing resources in the area, believing that the issue faced by people presenting complex needs is one of access rather than a large scale lack of resources.
As a Substance Misuse Link Worker seconded over from CRI, I work with a number of clients and provide flexible, creative, intensive support to enable each client to lead on and better navigate the pathway to their recovery. When clients are referred to the FLIC Team, link workers find out as much as possible about the difficulties they have had engaging with services in the past, and any barriers there have been to them getting the support they need, in order to work with them – and with services – to help change things in their future.
A CASE STUDY: PETER’S EXPERIENCE (5)
Summary of Issues
Peter is a 44-year-old Welsh male who was referred to the FLIC Team in October 2014. Peter moved to London at a young age and was raised in Islington. He left school at around age twelve with no qualifications. He is diagnosed with paranoid schizophrenia and has been previously been prescribed olanzapine (6), however at the time he misused this resulting in an overdose and an admission to Highgate Mental Health Hospital. Peter had a difficult upbringing; his mother was an alcoholic and he was brought up by his mother and his step dad. Peter has a number of convictions, mostly related to shoplifting, assaults, drunk and disorderly, racist abuse and breaches of ASBO (anti-social behaviour order). When referred to the team by Islington Outreach Team (a service helping rough sleepers), Peter was sleeping rough by the Canal in Camden, after being evicted from Camhurst House, a hostel in Islington. Peter has a long history of being in/out of various hostels in London, where on several occasions he was evicted due to his behaviour and inappropriate ways of dealing with others. He was a heavy drinker, drinking up to 4 litres of 7.5% cider daily as well as spirits, and refused support from services for his alcohol misuse. At the time of referral he was misusing drugs (mainly crack cocaine and cannabis) and on a prescription of 40ml methadone daily. Peter was socially isolated, with no constructive friendships or stable family.
Peter’s experience with the FLIC Team since being referred in October 2014
“I first met Nikki from the FLIC team when I was evicted from Camhurst House for having a pet mouse (“Mickey”) and playing loud music. I met Nikki and her colleague in a café on Holloway Road. I had no idea who they were, but I was told that I was referred to them by Islington Outreach team. I didn’t want to see anyone at the time. I was tipsy. I was here, there and everywhere. I was in a risky situation and close to death. I drank a lot at the time. Amaretto was like having a cuddle. It was like drinking anti-freeze. I slept out in the cold through Christmas 2014. I lit bonfires to cook by the canal. Wardens told me I couldn’t do this, as where I was lighting the bonfire there was an electricity box, but I still did what I wanted. On several occasions when I was drunk, I also fell into the canal only to find myself in hospital the next day.
Time passed. Islington Outreach Team & the FLIC Team (especially FLIC) tried helping me. I moved into three different temporary places and absolutely wrecked them. On one occasion, Nikki and her colleague from the FLIC Team were called out to come to get me from my temporary accommodation on Holloway Road because I was too drunk. When they arrived, all I can remember was someone lying at the other end of the bed. I was told I had to go somewhere (apparently to Housing Options), but I couldn’t get up and wouldn’t go anywhere. Amaretto had kicked in. I had a pet crab in the sink and water was overflowing. FLIC couldn’t do anything so they left. I was evicted, so I got another tent and slept out again. While on the street Nikki and her colleagues visited me to try helping me get off the streets and tackle my other issues.
Time passed and I was eventually placed in another temporary accommodation in Wood Green, with the help of the FLIC Team. Nikki helped me to change. She visited me in my accommodation on a weekly basis. She explained it was dangerous on the streets. Amongst many things, we met up for informal chats, spoke about my alcohol use, went to see my doctors and mental health services, sorted out my benefits and also spoke about my housing and long term goals. I was in Wood Green for about three or four months. I met people and made new friends. Once the area was new to me and I knew no one, I couldn’t get into trouble any more. Nikki kept supporting me and I couldn’t do it without her. Her visits cheered me up. Months down the line, Nikki told me I had done really well in Wood Green and hence it was time to move on. One day, Nikki turned up at my door in Wood Green, helped me pack, “kind of clean” and off we went to Ashley Road hostel (based in Finsbury Park, Islington).
To date, I’m still in Ashley Road, where I’ve been since around September 2015. I feel happy. I’ve calmed down a little bit and overall things are working well. FLIC made it ok. I know I still have my bad days and can fall back at times. I still drink whiskey and Amaretto because I have a bad toothache and I feel this helps, however overall my alcohol intake has decreased. Nikki keeps suggesting that I should go to see the dentist as drink isn’t a long term cure, but I’m scared to go. I am now on 30ml methadone, but shortly will be switching over to subutex. I don’t use illegal drugs any longer (except cannabis at times). My mental health is more stable and is being managed by my GP. I have been out of trouble with the police for over a year, which I feel is really positive.
I still have a long way to go. I still feel young, and look forward to moving into my own flat when/if that happens. I’m feeling good, trying to behave myself and do as much as I can.”
Footnotes
1 Al-Othman, H. (2016). Numbers of rough sleepers on London’s streets has doubled in five years. Available http://www.standard.co.uk/news/london/number-of-rough-sleepers-on-londons-streets-doubles-in-five-years-a3146721.html [24.01.16].
2 CHAIN: A multi-agency database recording information about rough sleepers that is commissioned and funded by the mayor of London’s office and managed by homelessness charity St Mungo’s Broadway.
3 Bramley, F. et al, commissioned by the Lankelly Chase Foundation (2015). Hard Edges: Severe and Multiple Disadvantage in England, Available http://www.lankellychase.org.uk/assets/0000/2858/Hard_Edges_Mapping_SMD_FINAL_VERSION_Web.pdf [24.01.16]
- February 8, 2016 No comments Posted in: Hot Topics Tags: Camden, Homelessness, Islington, Nikki Francalanza, fulfilling needs